Living with kidney disease and requiring regular dialysis treatments can be overwhelming enough without worrying about how to get to your life-sustaining appointments. For dialysis patients, reliable transportation isn’t just convenient – it’s critical for survival. Understanding your Non-Emergency Medical Transportation (NEMT) coverage options can ensure you never miss a treatment due to transportation barriers.
Dialysis patients typically need treatment three times per week, making transportation one of the most significant ongoing challenges they face. Fortunately, various insurance programs and resources are available to help cover transportation costs to these essential medical appointments.
Understanding NEMT for Dialysis Patients
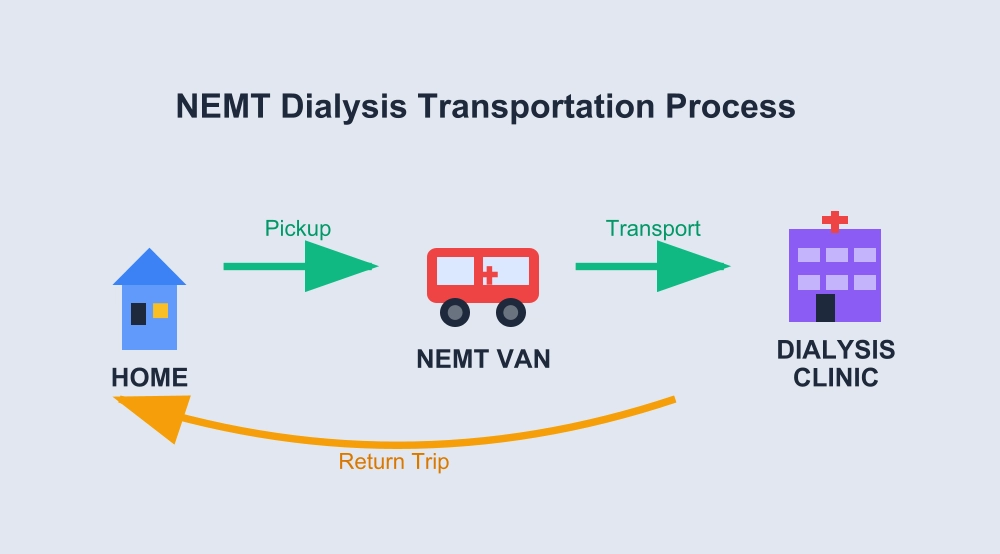
Non-Emergency Medical Transportation (NEMT) provides rides to medical appointments for people who cannot drive themselves or access other transportation. For dialysis patients, NEMT coverage is particularly important because treatments are frequent, predictable, and absolutely necessary for maintaining health and life.
Non-emergency medical transportation (NEMT) is a valuable service to individuals that require some help to transport them to/from their medical appointments. Such federal acknowledgment of the significance of NEMT also means that it is a reimbursed benefit by a variety of insurance plans, particularly in the case of dialysis patients, who have to undergo regular treatment.
Medicare Coverage for Dialysis Transportation
Medicare Part B and Dialysis
The Medicare benefits are generally effective on the first of the fourth month of your dialysis treatments. This 4-month waiting period will be calculated even when you have not enrolled in Medicare. This implies that the majority of individuals undergoing dialysis end up obtaining Medicare cover which comes with certain transportation benefits.
What Medicare Covers:
- Emergency ambulance transportation to dialysis facilities when medically necessary
- Non-emergency ambulance transport in specific circumstances
- Transportation when other forms of transport are contraindicated due to medical condition
What Medicare Typically Doesn’t Cover:
- Routine transportation to dialysis appointments
- Non-medical transportation services
- Transportation for patients who can safely use other forms of transport
Medicare Advantage Plans
Many Medicare Advantage plans offer enhanced transportation benefits beyond what Original Medicare provides. These plans may include:
- Regular transportation to dialysis appointments
- Wheelchair-accessible vehicle services
- Extended geographic coverage areas
- Coordination with local NEMT providers
Medicaid NEMT Coverage for Dialysis
Medicaid provides the most comprehensive NEMT coverage for dialysis patients. Some patients rely on Medicaid coverage during the 90 day period before Medicare can take effect. This coverage is critical for many ESRD patients across the nation.
Eligibility Requirements
To qualify for Medicaid NEMT for dialysis appointments, patients must:
- Be enrolled in Medicaid
- Have no other available means of transportation
- Need transportation to covered medical services (dialysis qualifies)
- Meet state-specific eligibility criteria
What Medicaid NEMT Covers
Transportation Types:
- Standard vehicles for ambulatory patients
- Wheelchair-accessible vans
- Stretcher transportation when medically necessary
- Specialized vehicles for patients with complex needs
Frequency:
- Recurring dialysis appointments (typically 3 times per week)
- Emergency dialysis sessions
- Related medical appointments (nephrology visits, lab work)
- Transportation to different dialysis facilities when medically necessary
Dual Coverage: Medicare and Medicaid
Many dialysis patients qualify for both Medicare and Medicaid (dual eligibles). This combination often provides the most comprehensive transportation coverage:
Medicare Primary: Covers dialysis treatment costs Medicaid Secondary: Covers transportation and other gaps in Medicare coverage
Dual eligibles typically have access to:
- Regular NEMT for all dialysis appointments
- Emergency transportation services
- Specialized vehicles when medically necessary
- Extended coverage areas
Employer-Sponsored Insurance
Some employer health plans offer transportation benefits, particularly for chronic conditions like kidney disease. Benefits may include:
- Reimbursement for transportation costs
- Contracted NEMT services
- Coordination with local transportation providers
- Flexible spending account eligibility for transportation costs
Kidney Disease-Specific Programs
Several organizations provide transportation assistance specifically for dialysis patients:
- American Kidney Fund transportation grants
- National Kidney Foundation local programs
- Dialysis center-sponsored transportation services
- Community-based kidney disease support programs
Step 1: Verify Your Coverage
Contact your insurance provider to confirm NEMT benefits:
- Call the customer service number on your insurance card
- Ask specifically about transportation to dialysis appointments
- Request information about approved NEMT providers in your area
- Understand any limitations or prior authorization requirements
Step 2: Get Prior Authorization (If Required)
Some insurance plans require prior authorization for NEMT services:
- Your nephrologist may need to document medical necessity
- Submit authorization requests well in advance
- Keep copies of all authorization documents
- Understand the duration of approved coverage
Step 3: Schedule Your Transportation
For Medicaid NEMT:
- Contact your state’s NEMT broker or coordinator
- Provide your Medicaid ID and dialysis schedule
- Schedule recurring appointments for ongoing treatments
- Confirm pickup times and locations
For Medicare Advantage Plans:
- Contact your plan’s transportation coordinator
- Verify which NEMT providers are covered
- Schedule appointments according to plan requirements
- Understand any copayments or limitations
Step 4: Prepare for Your Rides
What to Bring:
- Insurance cards and identification
- List of current medications
- Emergency contact information
- Comfort items for lengthy treatments
- Snacks or water (if allowed)
Timing Considerations:
- Schedule pickup 30 minutes before appointment time
- Account for potential delays
- Arrange return transportation
- Have backup transportation plans
State-Specific NEMT Programs
Transportation coverage varies significantly by state. Some states have particularly robust programs for dialysis patients:
Enhanced State Programs:
- Extended coverage areas for rural patients
- Specialized dialysis transportation fleets
- 24/7 emergency transportation services
- Coordination with dialysis centers
- Multi-language support services
Limited State Programs:
- Basic transportation to nearest dialysis facility
- Restricted scheduling options
- Limited coverage areas
- Reduced frequency allowances
Building Relationships
With Your Dialysis Center:
- Inform staff about your transportation needs
- Ask about center-sponsored transportation programs
- Request assistance with insurance authorization
- Coordinate appointments to minimize transportation needs
With NEMT Providers:
- Establish relationships with reliable drivers
- Communicate special needs or preferences
- Provide feedback to improve services
- Build backup provider relationships
Planning Strategies
Scheduling Efficiency:
- Group appointments on the same days when possible
- Request consistent appointment times
- Plan for holiday and weather disruptions
- Maintain flexible backup options
Cost Management:
- Understand your insurance benefits fully
- Keep receipts for potential reimbursement
- Explore grant programs for uncovered costs
- Consider tax deductions for medical transportation
Dialysis patients may face emergency transportation needs:
When to Use Emergency Services:
- Severe complications during treatment
- Unexpected health emergencies
- Transportation breakdown during treatment schedule
- Weather-related emergency situations
Emergency NEMT Options:
- Contact your NEMT provider’s emergency line
- Use backup transportation arrangements
- Contact your dialysis center for assistance
- Utilize emergency Medicaid transportation
Federal Resources
The Centers for Medicare & Medicaid Services give details about NEMT benefits and requirements. This official resource helps patients understand their rights and coverage options under federal programs.
National Organizations
The American Kidney Fund offers valuable information about dialysis costs and insurance coverage, including transportation assistance programs. They provide financial aid and advocacy resources specifically for kidney patients.
Additional Support Organizations:
- National Kidney Foundation local chapters
- Dialysis Patient Citizens advocacy group
- State kidney disease programs
- Local transportation assistance programs
Transportation Grants
Several organizations offer financial assistance for dialysis transportation:
- American Kidney Fund transportation grants
- Local kidney foundation programs
- Religious and community organization assistance
- Dialysis center hardship programs
Tax Considerations
Transportation costs for medical care may be tax-deductible:
- Keep detailed records of all transportation expenses
- Consult with tax professionals about medical deductions
- Consider using flexible spending accounts
- Understand IRS guidelines for medical transportation deductions
Long-term Transportation Strategies
Building Support Networks:
- Coordinate with family members for backup transportation
- Connect with other dialysis patients for ride-sharing
- Explore volunteer driver programs
- Consider relocating closer to dialysis facilities
Technology Solutions:
- Use ride-sharing apps that accept insurance
- Explore telemedicine for some appointments
- Utilize patient portal systems for appointment coordination
- Take advantage of transportation tracking apps
Learning about NEMT coverage to dialysis appointment is important to you and your health treatment schedule. Regardless of whether you are covered by Medicare and Medicaid or by a privately funded insurance program, transport options are available to assist you in getting life sustaining dialysis treatments.
The solution is to know your exact coverage and create connections with some trustworthy providers and always have a plan B in case of an emergency. Never allow transportation costs to be a hindrance to you getting the dialysis treatments that you require in order to sustain your health and quality of life.
For the most current information about your specific transportation benefits, contact your insurance provider directly and speak with your dialysis center’s social worker or patient coordinator. They can help you navigate the system and access all available resources to support your ongoing dialysis care.